|
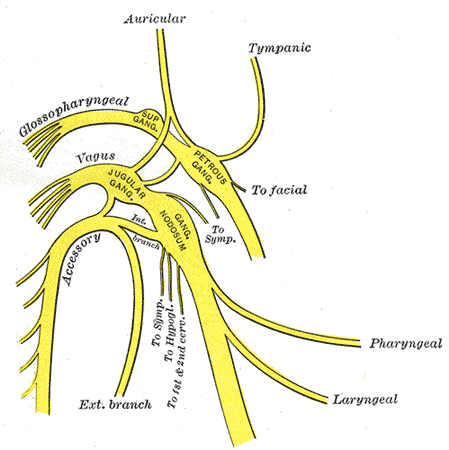
Chronic inflammation is a growing problem and is associated with myriad diseases including diabetes, heart disease, and cancer, to name but a few. In fact, back in 2004 Time Magazine had a cover story on inflammation, calling it "The Secret Killer." Inflammation is an adaptive process in our bodies, an evolutionary mechanism for survival. It is beneficial and necessary for our bodies to respond to stress, toxins, injuries, etc, but it needs to be in balance. If it continues without resolving, it can lead to chronic disease. The conventional approach is to block or suppress inflammation through the use of medications such as non-steroidal anti-inflammatory drugs (NSAIDs), commonly known as Advil or Ibuprofen. However, we now know that in order to heal we do not want to simply block inflammation, but rather modulate it to achieve balance and resolution. The field of psychoneuroimmunology studies how the brain interacts with the nervous system and immune function. It is a fascinating field, as this connection reveals how the mind and the way we think can actually influence and alter physiological processes, such as our immune response. This research also gives us potential non-drug treatments for inflammation and the conditions associated with it. A study published in January 2013 assessed the effects of mindful meditation on the inflammatory response. 49 participants were randomly assigned to either an 8-week mindfulness-based stress reduction program (MBSR) or an 8-week active control health enhancement program (HEP) that included walking, balance, agility, core strength, nutritional education, and music therapy. They then exposed both groups to psychological stress (public speaking) and physical stress (cayenne pepper rubbed on the arm), and found that the group trained in mindfulness-based stress reduction had significantly reduced post-stress inflammatory responses. This study showed that mindfulness-based meditation is able to alter the inflammatory response, but the mechanism was still largely unknown. One mechanism of meditation influencing inflammation is through the vagus nerve. The vagus nerve is large and far-reaching, with branches connecting to everything from the heart to the lungs and digestive tract. It's role in the immune response is referred to as the cholinergic anti-inflammatory pathway, and it explains how our thoughts and mind can directly influence the immune response and inflammation. It was first discovered in animal models that if you stimulated the vagus nerve it would reduce the release of inflammatory mediators. This has also been found in humans, and along with meditation, the vagus nerve can also be stimulated by aerobic exercise, acupuncture, and dietary supplements such as fish oils. A recent study from the University of Wisconsin showed that mindfulness-based meditation can actually affect the genes that control inflammation. The researchers measured the effects of a day of mindfulness-based meditation, and found altered levels of gene-regulating compounds and reduced levels of pro-inflammatory genes. These genetic and biochemical changes also correlated with faster recovery from a stressful situation.
If you suffer from an inflammatory condition such as arthritis or would like to prevent chronic inflammatory disease, there is good reason to consider non-drug treatments such as meditation and acupuncture to modulate the inflammatory response. Sources: Rosenkranz, Melissa A., et al. "A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation."Brain, behavior, and immunity 27 (2013): 174-184. Kaliman, Perla, et al. "Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators."Psychoneuroendocrinology 40 (2014): 96-107.
0 Comments
Leave a Reply. |
AuthorDr. Tomah Phillips, ND Archives
April 2020
Categories
All
|


 RSS Feed
RSS Feed